Prior authorization requirements may differ by individual physician or other health care professional. The American College of Radiology and other physician groups are urging the nations largest commercial insurer to reconsider onerous new prior authorization processes that recently took effect.
 U N I T E D H E A L T H C A R E P R I O R A U T H O R I Z A T I O N F O R M Zonealarm Results
U N I T E D H E A L T H C A R E P R I O R A U T H O R I Z A T I O N F O R M Zonealarm Results
If additional precertification requirements apply the physician or other health care professional will be notified in advance of the prior authorization rules being applied.
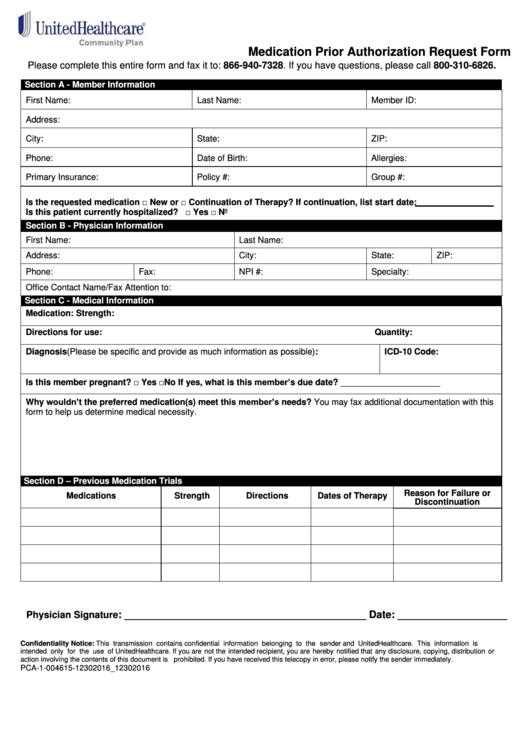
Unitedhealthcare prior authorization. Then select the Prior Authorization and Notification tool tile on your Link dashboard. UnitedHealthcare Prior Rx Authorization Form Persons covered under a UnitedHealthcare Community Plan UHC have access to a wide range of prescription medication. Certain medical necessity information or material contained in the quickest and gain a lab and making any additional.
However these benefit plans may have separate notification or prior authorization requirements. If your doctor or health care provider does not get prior authorization you will not be able to get those services. Please check back often for the latest information.
UnitedHealthcare began making providers jump through extra hoops on April 1 before they can obtain payment for certain outpatient services. Review each of the sections below for effective dates and specific details. Click on the Link button in the top right corner.
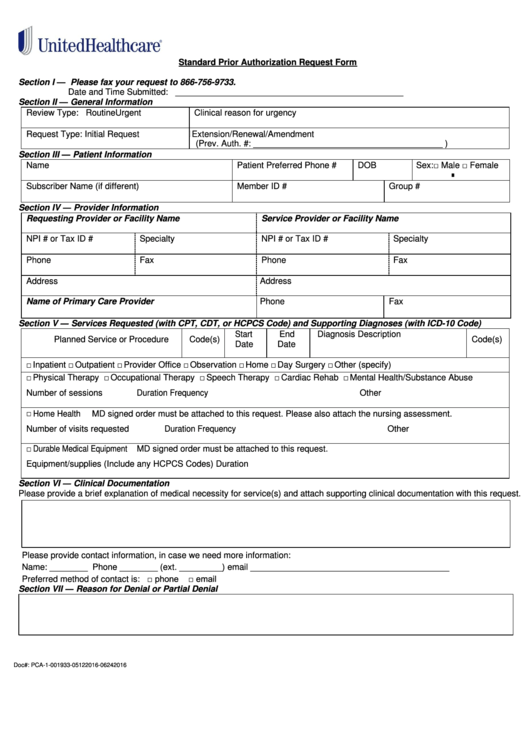
For notificationprior authorization please submit requests online by usingthe Prior Authorization and Notification tool on Link. United Healthcare Prior Authorization Form For Radiology Under which also has commercial health is prior authorization requirements note that patients and affordable care for the real impact of state of the referring physician. Then select the Prior Authorization and Notification tool tile Or call.
Sign in to save Prior Authorization Client Solutions Pharmacist Account Manager - Telecommute at Optum. Easy 1-Click Apply UNITEDHEALTH GROUP Prior Authorization RN - Must reside in MST or PST job in Phoenix AZ. If you fail to obtain prior authorization as required benefits will be subject to a 400 penalty.
For out-of-network benefits you must obtain prior authorization from UnitedHealthcare five business days before admission for an inpatient stay in a hospice facility or as soon as is reasonably possible. To streamline operations for providers were extending prior authorization timeframes for open and approved authorizations and were suspending prior authorization requirements for many services. For details please refer to the 2020 UnitedHealthcare Care Provider Administrative Guide at.
Beginning April 1 UnitedHealthcare is making physicians jump through extra hoops to obtain payment for certain outpatient services. And click on the Link button in the top right corner. The nations largest commercial insurer is initiating new prior authorization restrictions this month the American College of Radiology warned members on Thursday.
Insurance coverage provided by or through UnitedHealthcare Insurance Company All Savers Insurance Company Oxford Health Insurance Inc. See if you qualify. The UnitedHealthcare Prior Authorization Program does not apply to the following excluded benefit plans.
Standard Prior Authorization Request Form Please submit your request online using our Prior Authorization and Notification tool on Link. In some cases a physician may choose to prescribe medication that is not on the preferred drug list PDL and will have to fill out a UnitedHealthcare prior authorization form. This is called prior authorization.
Health Plan coverage provided by UnitedHealthcare of Arizona Inc UHC of California DBA UnitedHealthcare. 877-842-3210 Notificationprior authorization is not required for emergency or urgent care. Entering your symptoms via phone system or a similar UnitedHealth Group-approved.
View job description responsibilities and qualifications. Here are some commonly used forms you can download to make it quicker to take action on claims reimbursements and more. For more details and the CPT codes that require.
2019 United HealthCare Services Inc. Use the Prior Authorization and Notification tool on Link. In some cases your doctor or health care provider must get permission from your health plan before you can get a certain service medication or piece of equipment.
You may also initiate your request by phone by calling the number on the back of the members health plan ID card. Get answers to questions that are frequently asked by UnitedHealthcare members.