User IP address 10602059. The telehealth policy modifications outlined below were developed in consultation with regulators and clinical professionals throughout the South Carolina provider community.
Https Www Cms Gov Files Document General Telemedicine Toolkit Pdf
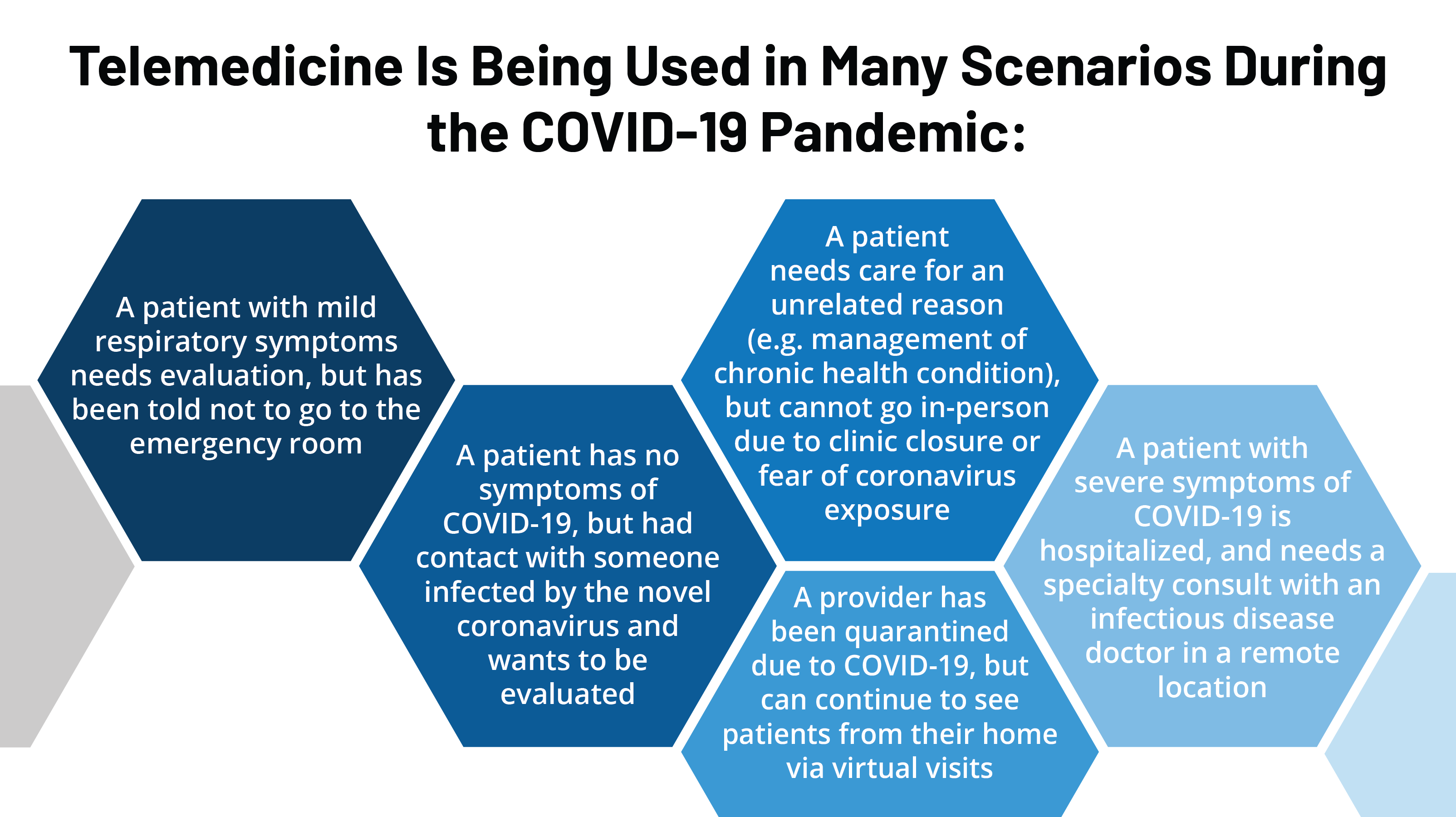
This can help minimize the spread of illness.
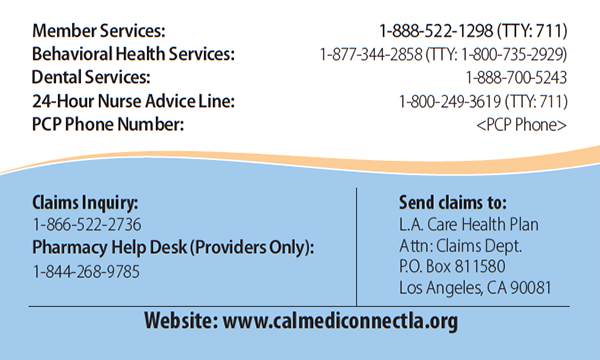
Sc medicaid telehealth. We are happy to announce the availability of the South Carolina Medicaid Web Portal. If you need help or have problems making your appointment call First Choice Member Services at 1-888-276-2020. Update your password Download or view payment e-remit statements online Enter and submit claims for Medicaid subscribers.
For information on South Carolina Medicaid reimbursement covered services and codes please visit South Carolina Healthy Connections Medicaid website. The South Carolina Telehealth Alliance SCTA is a statewide collaboration of many organizations joining forces to expand telehealth services across the state. The SCTA provides guidance assists with strategic development and advises on technology and standards to develop an open-access network.
Effective for dates of service on and after March 15 2020 SCDHHS is expanding coverage for telephonic and telehealth services. If you have questions call the Healthy Connections Medicaid Member Contact Center at 1-888-549-0820 from 8 am. This open-access network gives all South Carolina.
The patient clicks a link to sign up to be seen online by a provider who can refer them for drive-thru testing if needed at Doctors Cares Cayce SC location. As we continue to monitor the spread of COVID-19 we want to make you aware of expanded telehealth options available to our members. You may also call the South Carolina Department of Health and Human Services Fraud Hotline at 888-364-3224 or email fraudresscdhhsgov.
The medical care is individualized specific and consistent with symptoms or confirmed diagnosis of the illness or injury under treatment and not in excess of the beneficiarys need. Learn about health risks and get wellness tips. South Carolina Medicaid will reimburse for live video and covers telemedicine when the service is medically necessary and under the following circumstances.
For COVID-19-related telehealth services submitted to the fee-for-service benefit providers can elect to submit either 02 indicating telehealth or place of service code they would have used if the service had been provided in person FQHCs billing through the SCDHHS webtool should select POS 12. Providers engaging in telehealth are required to. This electronic communication means the use of interactive telecommunications equipment that includes at a minimum audio and video.
This system allows you to. Go to wwwS CDHHSgov. With telehealth you can consult with a health care provider without leaving your home.
State Laws and Policies. Medicaid South Carolina Medicaid reimburses for live video telemedicine and tele-psychiatry services. BSCPEC-1664-20 March 2020 Temporary telehealth coverage changes On Friday March 13 2020 President Donald Trump declared a national emergency due to.
Learn more about South Carolinas telemedicine policies with eVisit. Hover over the For Providers tab and click on Provider Manuals. No action is required by Medicaid members at this time.
To amend the code of laws of south carolina 1976 by adding section 44-6-38 so as to require the south carolina department of health and human services to reimburse practitioners for mental health telehealth services delivered to patients enrolled in medicaid. They are intended to balance immediate treatment needs that are not appropriate for deferral with the safety and efficacy of remote service delivery. See Rural Telehealth Services Document.
Medicaid MCOs may have additional. Private insurers have since fallen in line and many are covering telehealth treatment for mental health issues leaving only Medicaid recipients without full coverage. Visit the member portal to find out about your childs health needs.
Medicare Only applicable for rural areas at this time. If you need transportation to your appointment call the Medicaid Transportation Broker in your county. For purposes of Medicaid telemedicine seeks to improve a patients health by permitting two-way real time interactive communication between the patient and the physician or practitioner at the distant site.
The policy changes outlined below will remain in effect for the duration of the current declared public health emergency unless SCDHHS determines they should sunset at an earlier date. Be it enacted by the general assembly of the state of south carolina. Doctors Care is offering a telemedicine drive-thru option in South Carolina through its Doctors Care Anywhere Virtual Urgent Care app.
Policies differ from state to state so its important to be well informed. Existing Telemedicine Benefits Absolute Total Care will continue to follow the standard SCDHHS telemedicine benefit policies which is available to licensed physicians nurse practitioners and physician assistants as applicable. Telehealth lets you consult with a health care provider by phone or through video chats on your computer.
44-48 of the Medicaid Providers Manual.